Iraq’s preliminary Pfizer deal and covid-19 vaccine accessibility
This week Iraq signed a preliminary deal with USA’s pharmaceutical company Pfizer to receive 1.5 million doses of its covid-19 vaccine. Western officials stated that Washington urged Baghdad to choose the Pfizer-BioNTech vaccine over other options. Iraq committed 170 million dollar to close the deal, wanting to provide the vaccine for free to its citizens. However, as each person requires two injections of the vaccine, the order will cover only 750,000 of Iraq's 40 million people. This is, compared to for example Canada, a small number. Canada hoarded the world’s highest number of doses per person, ordering over 350 million vaccinations for a population of only 38 million people. This equates to nine doses per person. Additionally, the US signed an executive order telling the vaccine makers to prioritise Americans. Why is there such a big difference in purchasing capacity? Is one population more worthy of life than the other?

Several factors can be mentioned that impede the accessibility of the covid-19 vaccine. Ever since the scale of the pandemic became more severe, western governments began investing billions in Big Pharma to facilitate vaccine development. One must keep in mind that historically the development of vaccines – especially for active pandemics or epidemics – has rarely been profitable. The discovery process is slow, results are not guaranteed, and poor countries often require high supplies which they cannot afford. This was also why no vaccine had been developed for Zika or Ebola (the latter was only approved at the end of 2019) - as these diseases mostly affected poor parts of the world.
Priority access
The case of the covid-19 pandemic is somewhat different. When the scale of the crises became apparent, many NGO funds and bank loans, as well as countries’ governments like Canada ($180 million), Germany ($443 millon), UK ($84 million) and the US ($2.5 billion) invested in Big Pharma to help facilitate the development of a covid-19 vaccine. It was only then that the research & development race started. Given that this life-saving vaccine has been largely funded by the taxpayer, and relies on publicly funded science, one would think it would be made available to the public at no additional cost. However, Big Pharma is determined to receive substantial returns on their capital investment. Not only are these vaccines being sold for a profit, they are also being sold back to the governments that funded them in the first place – with the US, Canadian, British and EU governments securing hundreds of millions of doses. In other words: when these vaccines reach the public, they will have effectively been paid for twice. It also means that the billions of dollars handed over by the western countries to Big Pharma came with priority access at the cost of poorer or war affected countries. In the meantime, the lower purchasing power of low and middle-income countries caused many of them to leverage other means to acquire covid-19 vaccines. For example, Peru and South Africa volunteered to host clinical trials in exchange for vaccine doses. The absurd level of stockpiling of Western countries potentially spells disaster for non-western countries that have been pushed to the very back of the queue.
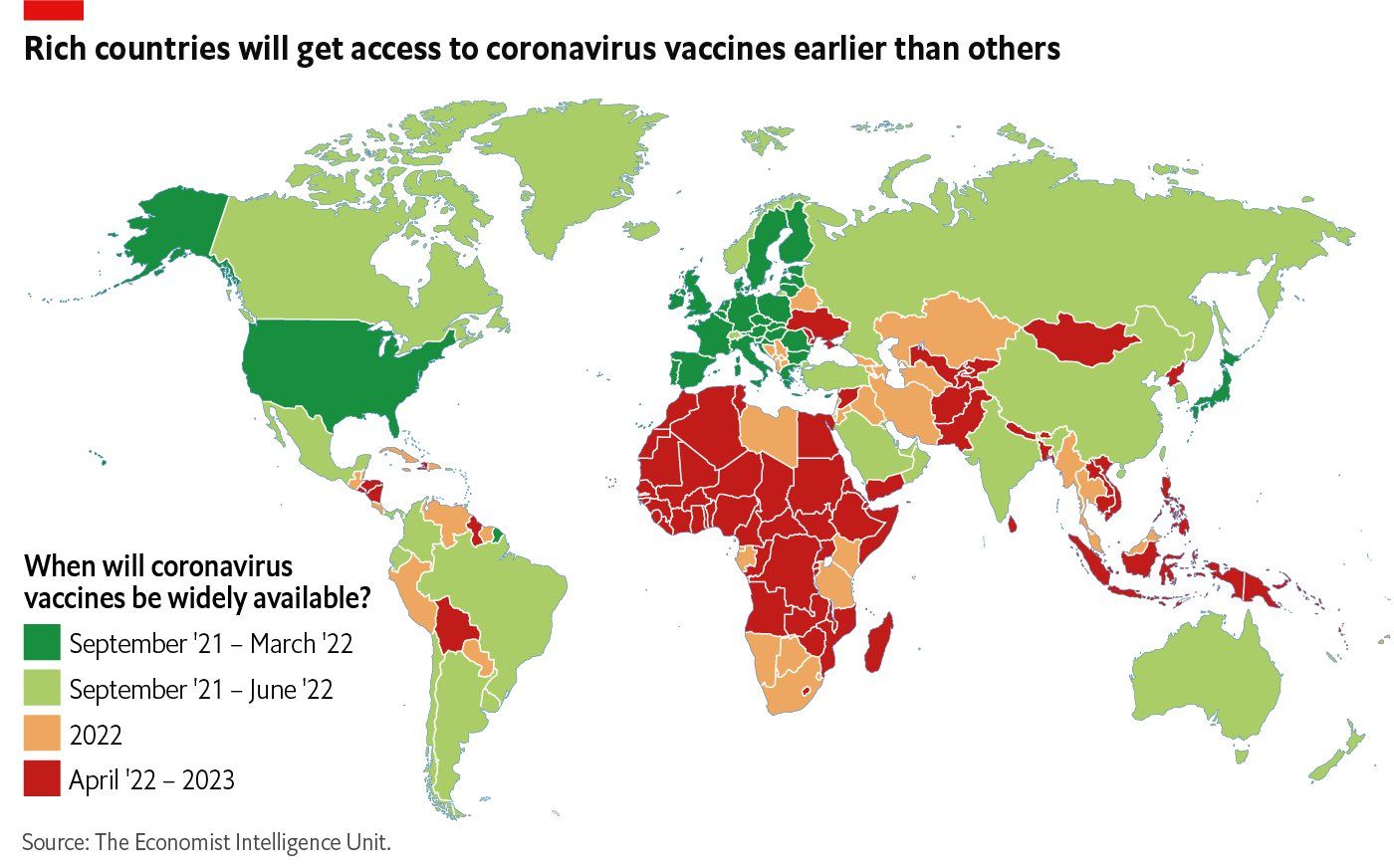
Western nations have reserved more vaccines than they actually need, and their developers will not share their intellectual property, leading to billions of people around the world not receiving a vaccine for covid-19 for years to come. The current system, where Big Pharma is using government funding for research and retains exclusive rights while keeping their technology secret to boost profits, will continue to cost many lives.
